Nepal’s National Suicide Prevention Helpline Service helping save lives

Every year more than 700 000 people die due to suicide globally. For every suicide, there are many more people who attempt to take their lives.
Almost 77 percent of suicides occur in low and middle-income countries
While suicide is a serious public health problem, it can be prevented with timely evidence-based, and often low-cost interventions including early identification of risk, assessing, managing, and follow-up of people exhibiting suicidal behavior.
Suicide deaths are strongly related to mental illness. The COVID-19 pandemic has had a severe impact on mental health and well-being of people globally. Apart from impeding access to mental health services, it sparked or amplified mental health issues both as a consequence of COVID-19 infection and from psychological distress, anxiety, and depression over the fear of illness or death including that of friends and loved ones, the extended periods of movement restrictions, social isolation.
Suicide reduction has been prioritized by WHO. In 2013 Ministers of Health of 194 WHO Member States adopted WHOs Comprehensive Mental Health Action Plan 2013-2020. The plan was extended until 2030 and sets out clear actions for countries with an aim to reduce suicide rates by at least one-third by 2030.
Fostering socio-emotional life skills in adolescents, limiting access to means of suicide, working with the media for responsible reporting of suicide, and early identification and management of the risk of suicide in healthcare and beyond are the four key interventions identified in WHO’s LIVE LIFE implementation Guide launched in June 2021 which supports countries by evidence-based strategies to prevent deaths by suicide.
In Nepal, according to a National Mental Health Survey in 2020, nearly 80 percent of people who need mental health care do not get it. According to data obtained from the Nepal police, the average annual increase in suicides over the past five years in Nepal is 7.2% which increased to 14% in 2021.
Annual deaths due to suicides in Nepal (Source: Nepal Police)
To address the issue, the Women and Social Parliamentary Committee directed the Ministry of Health and Population to take comprehensive action on suicide prevention.
Considering the severe absence of mental health services and resources for a large part of the population in Nepal, the WHO country office in Nepal in consultation with program managers, mental health experts, and civil society organizations, developed a concept paper with two strategic recommendations. The first is a short-term one to operationalize a National Suicide Prevention Helpline Service to provide crisis support- followed by a long-term strategy to establish a National Resource Center for suicide prevention in the National Mental Health Hospital to lead a multi-sectoral response.
As per the recommendations, the Ministry of Health and Planning (MoHP) agreed to establish the National Suicide Prevention Helpline Service at the Mental Hospital in Langankhel, Lalitpur, Nepal, the only government hospital in the country currently capable of treating patients with mental health issues.
On 10 September 2020, a dedicated four-digit phone helpline number ‘1166’ was obtained and became fully functional on 5 May 2021. While WHO provided technical and financial support to run the suicide prevention hotline service round the clock, the Transcultural Psychosocial Organization (TPO) Nepal provided operational support by recruiting and training counsellors and psychologists to answer the phones and counsel callers. TPO is also responsible for monitoring calls and maintaining records.

Workings of the suicide prevention helpline
Initially, four helpline responders were recruited and trained to provide crisis support for callers on the National Suicide Prevention Helpline Service. In the absence of a designated workspace at the Mental Hospital at Langankhel, Nepal, helpline operators (counsellors) at the Transcultural Psychosocial Organization (TPO) office were responding to the calls using mobile phones from their office premises initially. They shifted to the hospital premises when a physical workspace was identified. The Mental Hospital is also in the process of building a soundproof room with information technology (IT) equipment to provide a safe and confidential space to take calls and safely keep records.

A counsellor at the Suicide Prevention Helpline Center noting case details on while responding to a call on the National Helpline (Photo credit: WHO)
‘There are lots of things that can be done for suicide prevention, but we feel that the helpline is an entry point for people to enroll for the services. The people who call on the helpline give us power and motivation to work further in suicide prevention,’ said Parbati Shrestha, project coordinator at Transcultural Psychosocial Organization (TPO) Nepal
Since the helpline became operational in May 2021, it has received more than 3000 calls till March 31, 2022. Almost a quarter of the calls were related to suicide and other mental health issues. Callers shared their thoughts on suicide and their history of attempts.
For callers determined to be at immediate risk of suicide, crisis management is done with the callers requested to keep away from the means they have chosen. Callers are also requested not to be alone and to be with any friends or family. As per the risk involved or depending on the gravity of the situation, counsellors also talk to family members and other individuals who may have a significant role in the lives of the callers. If there is a high risk of suicide, the police are also requested to initiate a rescue.
‘I am thankful for the helpline service because it made me aware of a lot of emotional issues that I was going through. This facilitated me to visit the doctor after I tried to end my life,’ said a 25-year-old woman caller who wished to remain anonymous.
Follow-up calls are also made, and the callers are invited for counseling and health support. In some of the cases, counsellors also facilitate doctors visit for the callers.
‘After dealing with hundreds of calls wherein people talk about how they want to end their lives, I feel I have become more empathetic, though it can emotionally drain you out,’ said 30-year-old Manil Maharjan, a resident of Kathmandu who lost one of his college batchmates to suicide and has been working closely with a suicide prevention helpline in Nepal. Maharjan adds, ‘If one can play even a small role in convincing someone to not give up on life, there can’t be a more satisfying job than that. This is the job I have been waiting for all my life.’
For callers seeking information regarding other mental health issues, counsellors provide psycho-education and systematic explanations about the disease. In case the caller prefers to chat via text messages rather than talking over the helpline, counsellors support them by engaging with them through text chat as well. Extended counseling services are also provided to Outpatient Department (OPD) referrals, helplines, and other service providers.
With an aim to normalize the seeking of mental health services and support, orientation programs were conducted with youth in schools and colleges. This was done as adolescents and youth are at a critical phase of acquiring socio-emotional skills and face the risk of the onset of mental health conditions. Various informative videos on mental health were prepared and disseminated as part of the orientation programme.
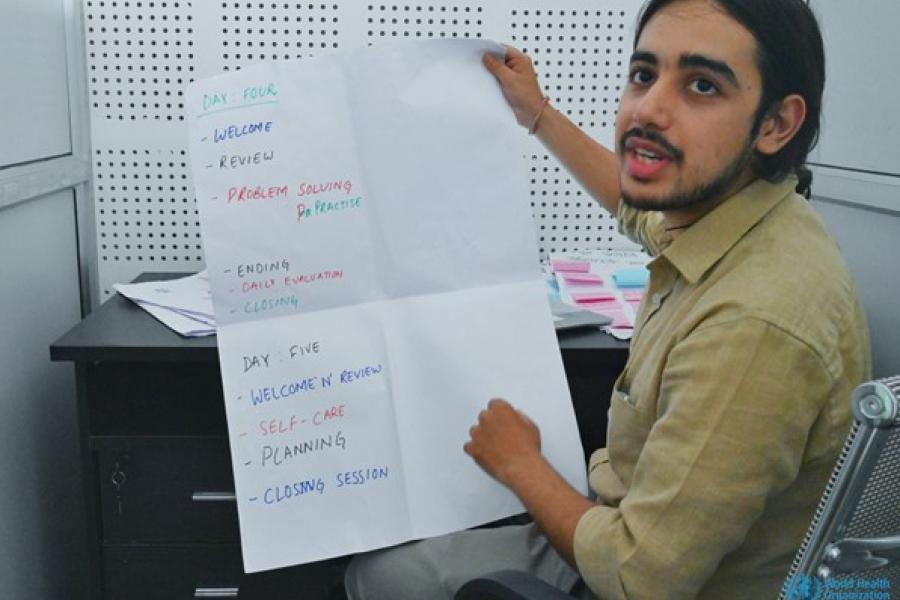
To maintain uniformity of support, Standard Operating Procedures (SOPs) were also developed during this project in consultation with various experts in the field of mental health and psychiatry. With support from WHO, team coordination and training were carried out for the helpline operators to ensure smooth referral and case management
Establishing a national resource centre and expanding mental health services

The Mental Hospital, Lagankhel, Nepal where the Suicide Prevention Helpline Center is located (Photo Credit: WHO)
The mental hospital in Lagankhel, Nepal with support from WHO is in the process of establishing a national resource center for suicide prevention in the country to serve as a hub for technical innovation and multisectoral collaboration.
Additional features are being added to the helpline which is being expanded through the digital platform. The inclusion of social media tools such as chatbots and messenger calls are being incorporated. The aim is to expand coverage of the helpline and make it easier for individuals who are hesitant of calling and would prefer to connect via text messages or chatbots. It will also enable individuals living outside the country to reach out for support online.
As part of WHO’s LIVE LIFE Implementation guide for suicide prevention in countries, the resource center is expanding multisectoral work.. The WHO guideline on responsible media reporting on suicide has been adapted to give a national context. A media orientation package is being developed and the content has been translated into Nepali. Work has also begun with the agricultural ministry to regulate the availability of pesticides in the country. As part of the suicide prevention initiative, a prototype suicide registry has been drafted with a plan to pilot it in the coming months. The dedicated registry is expected to provide epidemiological information on suicide in Nepal which is critical to service planning and organization.
All these initiatives are an important priority in the National Mental Health Strategy and Action Plan 2020 and the draft National Suicide Strategy being developed by National Planning Commission.
Optimizing the helpline
The helpline number has still not been fully optimized yet. Available data on the ratio and pattern of calls received on the helpline show that more awareness needs to be generated among people about the availability of the national helpline and to build trust. To increase awareness and reach, messages promoting the helpline are being relayed on social media, radio, and television channels.
Currently, there is no calling charge for callers using the national telecom operator to access the national helpline, standard calling rates apply if callers use the services of private telecom operators. To overcome this, the call center is in the process of adapting the helpline to make it accessible online. This will also enable Nepalis living overseas to seek support.
While a lot more remains to be done, the National Suicide Prevention Helpline Service and the initiatives to further strengthen mental health services in Nepal are a step in the right direction towards ensuring equitable access to mental health services so that everyone can get the support they need to realise their abilities and mental wellbeing.

